Cushing’s disease, also known as hyperadrenocorticism, occurs when the adrenal glands or adrenal cortex overproduce cortisol. This hormonal imbalance affects many body functions and can lead to clinical signs such as a pot-bellied appearance, hair loss, increased drinking and eating, and changes in body condition. The diagnosis begins with diagnostic tests like blood tests, urine testing, and imaging—such as ultrasound—to identify problems with the adrenal glands or adrenal glands. A veterinarian will use these results to confirm disease and decide on the best treatment plan.
Treatment options aim to manage the disease and regulate cortisol levels. The most common therapy is medication that suppresses hormone production or replaces hormones when there is cortisol deficiency. Medication management often involves hormone suppression or hormone replacement to balance cortisol and cortisone levels. For some cases, especially when a tumor on the adrenal gland is overproducing cortisol, surgical removal of the adrenal gland—called adrenalectomy—may be the best option.
In my experience, veterinary medicine has made great advances in disease management. When dog owners follow a carefully designed treatment strategy, including regular veterinary care and disease monitoring, the prognosis can be quite positive. Hormone therapy and medical treatment can help control clinical signs and improve your pet’s quality of life. In some cases, surgical removal can provide a cure, but ongoing health assessment and disease monitoring are essential to ensure long-term pet wellness.
Common Types
Cushing’s disease, also called hyperadrenocorticism, happens when the adrenal glands or pituitary gland overproduce hormones like cortisol. This hormonal imbalance affects many body functions and causes clinical signs such as a pot-bellied appearance, hair loss, increased drinking and eating, and changes in body condition. To find out if a dog has this disease, a veterinarian will do blood tests, ultrasound, or other imaging like CT or MRI. These lab tests help with diagnosis and disease classification.
Once the diagnosis is confirmed, treatment aims to manage the disease and regulate cortisol levels. Medical treatment often involves hormone therapy which suppresses hormone production or replaces hormones if there is a cortisol deficiency. In many cases, medication can help control excess cortisol and improve clinical signs. Sometimes, a surgical removal of the adrenal tumor or pituitary tumor—called adrenalectomy or pituitary surgery—is necessary, especially if there is a benign mass or adrenal mass causing the problem.
In my experience, veterinary medicine provides effective treatment options for pets with Cushing’s disease. The success of treatment depends on understanding whether the disease is pituitary-dependent or adrenal-dependent. Disease management involves ongoing health monitoring and clinical evaluation to adjust therapy options and ensure pet wellness. With proper veterinary intervention, dogs can often enjoy an improved quality of life despite this life-threatening disease.
Signs of Cushing’s Disease
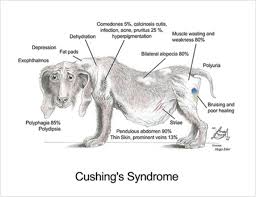
Cushing’s disease often develops slowly, especially in middle-aged or older dogs. The clinical signs can be subtle at first, making it hard to notice early on. Common signs include increased thirst, increased urination, and increased appetite, which are often the first symptoms owners see. As the disease progresses, the dog may become lethargic, show lack of activity, and have a poor hair coat. Many pets also develop a pot-bellied abdomen with enlargement of the abdominal organs and fat deposits that cause a stretching of the abdomen and abdominal wall.
Other clinical signs include fragile skin, hair loss, and recurrent skin infections such as pyoderma. The skin may also show hyperpigmentation, skin mineralization, and calcinosis cutis—hardening or calcification of the skin. Pets with Cushing’s often pant excessively, have poor skin healing, and may develop signs of muscle atrophy in the body. Some dogs may also develop bladder infections or recurrent skin infections, adding to their health concerns.
From my experience, recognizing these signs early can greatly help in diagnosis and treatment. The clinical signs are often mistaken for aging or other health conditions, but if you notice a pot-bellied appearance, excessive panting, or recurrent infections, it is important to seek veterinary care. Proper health assessment and clinical evaluation are essential steps to confirm hyperadrenocorticism and start effective disease management.
Treating Cushing’s Disease
Most veterinarians start treatment by diagnosing whether the disease is pituitary-dependent or adrenal-dependent. For adrenal tumor cases, surgical removal of the adrenal gland or adrenalectomy is often recommended. However, surgery carries risks like bleeding, infection, or adrenal destruction that can sometimes lead to death. In pituitary-dependent cases, medications are usually used to manage cortisol levels. These medications include drugs like Vetoryl (trilostane), which is FDA-approved, or Lysodren (mitotane). These drugs work by balancing hormone production and inhibiting cortisol synthesis in the adrenal glands.
Treatment management requires lifelong monitoring with blood tests and blood work to check the response to medications. The dose of drugs like Vetoryl often needs adjustment based on test results to prevent side effects such as sodium imbalance, potassium imbalance, or other serious reactions like bloody diarrhea or collapse. Side effects can sometimes be severe, so veterinarians carefully report and manage any drug reactions. In some cases, radiation therapy can be used to treat pituitary tumors or adrenal tumors that are malignant or non-malignant.
In my experience, treatment is often a balancing act—aiming to control cortisol production while maintaining a good quality of life. Medications like Anipryl (selegiline) are off-label options but can be helpful in specific cases. Diet can also support treatment, with low-fat options from brands like Royal Canin or Hill’s Prescription Diet. Sometimes, surgery or radiation therapy might be needed if tumors recurr or are malignant. The goal is to manage the disease effectively, minimizing side effects and complications while monitoring the animal’s health closely.
What Is Cushing’s Disease in Dogs?
Cushing’s disease, also known as canine Cushing’s syndrome, is an endocrine disorder that mainly affects middle-aged and senior dogs. It happens when the adrenal glands or pituitary gland develop problems that cause the body to produce too much cortisol, a steroid hormone. Normally, cortisol helps the body respond to stress and regulate many body functions. The pituitary gland, located in the brain, stimulates the adrenal glands to produce hormones through adrenocorticotropic hormone (ACTH). But in Cushing’s disease, a faulty feedback mechanism causes the glands to continue producing cortisol even when it isn’t needed, leading to hyperadrenocorticism.
If untreated, symptoms like increased thirst, excessive panting, and hair loss can reduce the dog’s quality of life. This disorder can be caused by pituitary tumors or adrenal tumors. The pituitary tumor signals the adrenal glands to produce too much cortisol, which affects many body functions. Because of this, treatment becomes very important to manage the disease and prevent serious complications such as adrenal destruction or death.
Based on my experience, treatments include medication, surgery, or radiation therapy. Many dogs respond well to medication like Vetoryl (trilostane), which is FDA-approved and stops cortisol production. However, side effects such as bloody diarrhea, collapse, or sodium and potassium imbalances can occur, requiring monitoring with blood tests. Sometimes, surgery to remove pituitary or adrenal tumors is necessary, especially in malignant or non-malignant cases. A balancing act exists in management, aiming to improve the dog’s health while minimizing side effects. Proper care with vet guidance helps to maintain a good quality of life for dogs with Cushing’s disease.
What are Symptoms of Cushing’s Disease in Dogs?
Cushing’s disease in dogs can show many symptoms that owners might notice. One common sign is panting that seems more than normal, even when it’s not hot or active. Many affected dogs will also eat and drink more than normal. Keeping track of how much food and water your dog consumes each day can help determine if these symptoms are linked to Cushing’s disease. Using an automatic feeder or measuring the portions of meals can help ensure your dog is eating per day in a consistent way. Similarly, measuring water intake daily by monitoring the water bowl can give clues about increased drinking.
Other symptoms include a potbelly appearance and weight loss with lethargy. Many dogs with Cushing’s disease develop thin skin and hair loss, which can make their skin look calcified or hardened. You might also notice skin infections or hard lumps underneath the skin that are signs of growth caused by hormonal imbalance. These physical changes often progress slowly but are important to report to your veterinarian for proper management. Recognizing these symptoms early can make a big difference in treating the disorder and helping your dog maintain a better quality of life.
From my experience, understanding how cortisol influences behavior and appearance helps in early diagnosis. Monitoring symptoms like panting, increased eating and drinking, and skin changes can lead to timely treatment and better management of Cushing’s disease in dogs.
What Causes Cushing’s Disease in Dogs?
Cushing’s disease in dogs often develops when the pituitary gland produces too much ACTH, leading to overproduction of corticosteroid hormones by the adrenal gland. It can also be adrenal-dependent, caused by tumors on the adrenal glands. In my experience, many cases are diagnosed through a combination of blood sample testing and imaging. A common testing method involves measuring resting cortisol levels to see if they are normally within range or increased.
One test that is least expensive and widely used is the dexamethasone suppression test. During this test, drug dexamethasone is administered through a vein, and additional blood samples are collected after four and eight hours to measure cortisol levels. If the levels are suppressed, it suggests Cushing’s disease caused by pituitary issues. If not, it could be adrenal-dependent. In my clinical practice, this test helps determine the cause of the disease and guides the best treatment options.
How Veterinarians Diagnose Cushing’s Disease in Dogs
As a veterinarian, I often begin with a thorough physical exam and ask the owner to mention any symptoms that present themselves around the time started. To diagnose dogs with suspected Cushing’s disease, I recommend diagnostic testing such as the low-dose dexamethasone suppression test and the ACTH stimulation test. These tests help diagnose whether the dog has Cushing’s disease by showing how the body responds to certain medications or hormones. Sometimes, I need to prescribe medications or perform additional tests like blood work or imaging to confirm the diagnosis and determine the cause. Based on these results, I can develop the best treatment plan for the dog’s health.
Low-dose Dexamethasone Suppression Test
The low-dose dexamethasone suppression test is a common testing method used to help diagnose canine Cushing’s disease. During this test, a blood sample is taken to measure the resting cortisol levels before a drug called dexamethasone, a corticosteroid, is administered through a vein. After giving the drug, additional blood samples are collected at four and eight hours to measure how the cortisol levels change. Normally, the cortisol should be suppressed or decreased significantly, but in dogs with Cushing’s, the levels often increase or fail to reduce. This testing method is considered the least expensive option and provides clear results that help support the diagnosis. In my experience, this test is very useful because it gives quick results and is easy to perform.
ACTH Stimulation Test
The ACTH stimulation test is a common way to assess canine Cushing’s disease. During this test, a blood sample is taken to measure resting cortisol levels before administering synthetic ACTH. After the injection, blood is drawn again to measure the cortisol levels to see if they increase as expected. If the cortisol levels do not rise appropriately, it can help differentiate whether the disease is pituitary-dependent or adrenal-dependent. This test is very useful because it gives a quick picture of how the body responds to ACTH.
In my experience, the ACTH stimulation test is often combined with additional tests such as the high-dose dexamethasone suppression test and imaging like abdominal ultrasound, CT, or MRI to identify tumors or abnormalities in the adrenal glands. Sometimes, blood work showing high cholesterol, triglycerides, or altered white blood cells and dilute urine can support the diagnosis and overall health assessment. This comprehensive approach helps support a clear diagnosis and guide effective treatment plans.
Management of Cushing’s Disease in Dogs
Managing Cushing’s disease in dogs involves careful monitoring and proper use of steroid medications. Once your dog is diagnosed, your vet will create a treatment plan that includes dosing the medication at the appropriate level. This is very important because excessive medication can cause clinical signs like excessive thirst and other issues. Regular appointments are crucial so the vet can notice any change in your dog’s condition or symptoms and adjust the medication dosage if needed.
The main goal is to keep the disease controlled and prevent further development of pituitary or adrenal tumors. It’s important to follow the vet’s guidelines closely and monitor your dog’s response through blood work and ACTH stimulation tests. Iatrogenic conditions, caused by dosing too high or too low, can develop if the medication is not carefully managed.
In my experience, staying vigilant for signs like returning symptoms or increased thirst helps catch issues early. If you notice any change, especially if your dog seems more lethargic or appetite changes, you should contact your vet immediately. Proper management with regular blood tests and follow-up ensures your pet stays healthy and symptoms are controlled for the rest of their life.
How is Cushing’s disease diagnosed?
To diagnose Cushing’s disease in dogs, a veterinarian will start with a thorough examination and a review of your pet’s history. This helps establish a baseline and look for signs that suggest the disease. The vet will then perform blood tests such as a complete blood count (CBC) and biochemistry profile to check for abnormalities like elevated liver enzyme levels, especially ALP, or changes in white blood cell numbers that could indicate stress or other issues. Urine testing is also helpful; it can reveal elevated urine concentration or abnormal protein levels, which are common signs of Cushing’s.
Additionally, imaging techniques like X-rays and ultrasound of the abdomen are used to look for an enlarged liver or adrenal glands that might be noted as enlarged or tumors. These tests can help identify if the adrenal glands are abnormal in size or shape. To confirm the diagnosis, blood tests such as the ACTH stimulation test and low-dose dexamethasone (LDDS) test are necessary. High-dose dexamethasone (HDDS) test and urine cortisol:creatinine ratio are also used to determine the presence of Cushing’s and help predict the prognosis. Although some tests can be expensive, they are necessary to accurately diagnose Cushing’s disease and plan effective treatment.
From my experience, combining laboratory testing with imaging gives a clearer picture of the disease. These tests help confirm the diagnosis and determine the best treatment options for your pet. I often provide a handout on “Cushing’s Disease: Testing” to pet owners so they understand the importance of each step in the diagnostic process.
What do I need to know if my dog’s disease is being managed with medication?
When your veterinarian creates a treatment plan for your pet’s condition, it’s essential to follow their guidelines closely. The success of treatments often depend on the consistent and regular administration of the medication. For dogs with Cushing’s Disease, lifelong treatment may be necessary to keep the condition under control. Most dogs can be successfully treated with few medication side effects, but they must be carefully monitored using blood tests and clinical signs.
It’s important to do follow-up blood tests to ensure your dog is receiving the proper dosage—not too little or too much of the drug. Both can lead to complications. Proper dosage is crucial because an incorrect amount can cause side effects or reduce treatment effectiveness. My experience with pets on medication shows that regular check-ups and blood tests help catch issues early, ensuring your dog remains healthy and comfortable during treatment.
What is the prognosis?
Your veterinarian will outline a treatment plan for your pet’s condition. Be sure to follow their guidelines closely because these treatments depend on consistent and regular administration of the medication. Lifelong treatment may be necessary. Most dogs can be successfully treated with few medication side effects. However, your pet must be carefully monitored using blood tests and clinical signs. Follow-up blood tests are very important to be certain your pet is receiving the proper dosage and not too little or too much of the drug, both of which can cause complications.

Pingback: Why Won't My Dog Stop Shaking His Head: Should I Worry?
Pingback: Dog Parents Alert: First Aid for Broken Nails Revealed